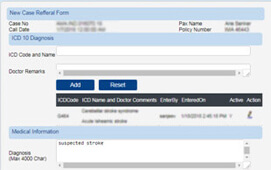
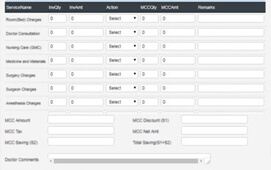
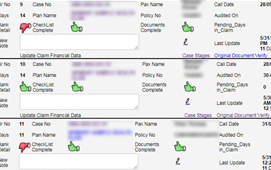
MedinyX is a complete TPA (Third Party Administrator) solution for claims management system. It is designed to enable automated health benefits administration and claim adjudication. An improved user experience, improved patient care standards, significantly reduced administrative costs, and much more can all be achieved while adhering to all regulatory standards.
Our product can easily adapt to any existing infrastructure. The software can be customized with any third-party application to meet the market's ever-changing demands.
MedinyX TPA Claims Management System offers influential advantages to enhance the velocity and effectiveness of claims preparation and settlements further escalating client administration and fulfillment levels.